 Cedric Yu, GammaPod inventor and founder of Xcision Medical Systems, LLC, talks about how an idea to create a more convenient radiotherapy technology came about—and how the GammaPod is now available to women with breast cancer.
Cedric Yu, GammaPod inventor and founder of Xcision Medical Systems, LLC, talks about how an idea to create a more convenient radiotherapy technology came about—and how the GammaPod is now available to women with breast cancer.
The idea of a better radiation treatment for women with an early breast cancer diagnosis came quite early, when I was at William Beaumont Hospital in Detroit, Michigan from 1992-1997.
During that time, we were treating many early-stage breast cancer patients and saw the impact of the time needed for treatments. Patients of an older age had to drive themselves, sometimes for a few hours, to the clinic every day or be driven by their children or somebody else. Also, you have younger woman with children, with a job. After surgery and 6-8 weeks of wound healing, the patient received 25 to 33 daily radiation treatments. So, altogether, from surgery to finished radiation treatment, we’re talking about a few months.
Women are busy and it’s a very difficult time. So, at that time, we provided a quick three-day treatment, essentially either using interstitially high dose rate brachytherapy, introducing seeds inside by a machine or we built iodine source chains and manually put them into the breast—and then, after a few days, manually took them out. Those are not small tubes, and it was just so brutal and painful to look at.


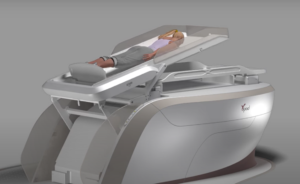
Seeds with brachytherapy (above) vs. GammaPod (below) where the patient is in the prone position on the treatment table with the breast in a stereotactic breast cup system.

We all know that, in the western world, most patients are diagnosed early. More than 60% are in a category called T1N0M0, which is a tiny tumor, and the nodes are negative and non-metastatic. And for such a small tumor, a woman is still subject to a surgery and so much pain.
“At that point, I thought, “There has to be a better way of doing this.”
So, I thought, “Well, maybe radiosurgery could be an option, just like the Gamma Knife for the brain. Maybe using the same concept and applying it to the breast could make the entire treatment easier.”
Taking the Idea to Reality Took Patience
For most early-stage breast cancer diagnoses, I begin to think that surgery would not be necessary if there was a more dedicated radiation option. Patients could have a single treatment and then go home and take tamoxifen or other medicine as indicated. And it would result in the best cosmetic results, be non-invasive with no pain, no anesthesia, and no scars to remind her what she has gone through. That was basically the driving idea to develop the GammaPod.
I applied for a grant for developing the idea in 1996, but I didn’t get it. My grant application was not even scored. I was also a grant reviewer at that time, so I knew that if your grant is unscored, it’s a clear message, “Don’t come back”. So, I didn’t resubmit right away.
Ten years later, I looked at the breast cancer treatment landscape and the same problem persisted. I thought, “Well, the idea is still valid, and I should pursue it”. So, that’s how the whole thing got started. The next time I applied for a grant, I got it the first round.
What Sets GammaPod Apart
What differentiates GammaPod versus other radiation machines is simple. Consider this analogy: it’s very difficult to come up with a shoe that you can run in and wear to a Presidential Ball. If you have such a shoe you can wear to both, it most likely must compromise one way or the other.
A dedicated machine to a specific disease does not compromise for that disease vs. a machine that treats many diseases, head to toe.
 The typical linear accelerator/external beam treatment for breast uses tangential fields. The word “tangential” means that the lower border is a straight line, tangent to the chest wall. Our chest wall is not a straight line, but curved, and part of the lung and heart will be in the beam.
The typical linear accelerator/external beam treatment for breast uses tangential fields. The word “tangential” means that the lower border is a straight line, tangent to the chest wall. Our chest wall is not a straight line, but curved, and part of the lung and heart will be in the beam.
With GammaPod, we treat in prone position, with the breast immobilized beneath the patient’s support couch. In this way, breathing has no effect whatsoever on the target and this allows us to treat more accurately. When you set the patient in supine position, without an accurate way of immobilizing the breast, you cannot guarantee that the patient is set in the same manner from day to day, because the breast is a pliable organ. The entire breast and chest wall will also move during the treatment because the patient breathes.
I can confidently say that no matter if a radiation oncologist uses protons or photons, there’s nothing in the world that can produce a dose distribution that’s more conformal than GammaPod.
Clinical Trials Showing a Positive Future
Traditionally, radiation treatment is given after surgery, or post-operatively. Our GammaPod users started with 5 treatments, rather than the traditional 15 or 16 treatments and saw lower toxicities. Now, they mostly use a single GammaPod treatment – with even lower toxicity to achieve similar clinical results.
Clinical trials to assess the feasibility of eliminating surgery are also being conducted. With a single ablative dose given before surgery with the GammaPod, it was reported that there were no active tumor cells in more than 93% of the surgical specimen when the surgery is performed months after the GammaPod treatment. These results will change the standard of care for the treatment of early-stage breast cancer.
Patients Want Convenient and Non-Invasive Treatments—and Confidence in Accuracy
Many women tell me they fall asleep during their GammaPod treatment—10, 15 minutes and they’re done. How nice is this for a woman’s treatment for cancer?!
On the day of treatment, the patient will receive a three-dimensional imaging, and, after that, the plan will be developed, and the patient will be treated based on today’s anatomy. That ensures the highest accuracy for delivering a treatment to the patient. Because we’re delivering a very high dose, you better deliver to the right perfect location—and that’s what the whole workflow is designed around.
GammaPod was optimized for treating early-stage breast cancer and as an inventor of this machine, I’m so happy that it has been benefitting many patients. It is the only machine that you can use to deliver a very high radiation dose pre-operatively to test the feasibility of eliminating surgery or a single post-operative treatment as an ultra-accelerated partial breast irradiation.
“It’s ultimate precision and I do believe that this will change how early breast cancer is managed. Hopefully, someday, having breast cancer will not be so scary anymore.”
If you look at the history of breast cancer care, it has always been moving towards minimizing the trauma to the patient—from radical mastectomy to lumpectomy plus 30-some treatments and now 15 treatments. So, looking at that evolution, we are working in the right direction.
Another important fact to note is that medicine—today’s medicine—is also more effective. And with the more effective medicine, we should be able to lessen the local, regional treatment, to make the local, regional treatment less invasive and more convenient for the patient.
“If there is one message that I want to give, it would be my gratitude to all the patients who willingly participated in the trials that our clinical collaborators are conducting. They are the true pioneers working toward the goal of improving care for other women in the world.”
